Your Family Deserves the Best Care Book an Appointment
Your skin health matters, so don’t delay. Our clinicians look forward to treating you and your family at one of our local New England practices.
Find Your Nearest APDerm Center
Melanoma is a scary word to hear. Most people know that melanoma can be a deadly skin cancer and often know someone close to them who has had melanoma. Many of my patients ask what they should be looking for to make sure a brown spot is not a melanoma. In this post, I will discuss when to be concerned that a growth could be a melanoma, how melanoma is diagnosed, and what treatments are available.
Most people know that melanomas are typically a dark or unusual looking brown spot on the skin. Concern for melanoma is a common reason that people come in to see the dermatologist or are referred to the dermatologist by their primary care physician – or are dragged to the dermatologist by a family member. The reason is often a new brown spot, a changing brown spot, or a bleeding spot. These are all excellent reasons to see the dermatologist!
When you come in to see me for a mole of concern, I will want to look carefully at that mole. And I will want to look over the rest of your moles to see how that mole fits in with its “cousins.” When I look at the mole of concern (and the rest of your moles), I will be applying criteria in my mind that you can also apply at home, though my colleagues and I have a little more experience to go on.
Concerning Features
When we talk about melanomas or concerning moles, we talk about the ABCDEs of melanoma: Asymmetry, Border irregularity, different Colors in one mole, Diameter greater than 6m, and Evolution. Let me go through them one at a time.
Asymmetry refers to the overall pattern of the mole. If you cut the mole in half, it means one side will look different from the other.
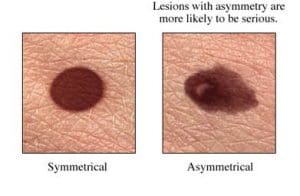
Mole (A) on the left is very symmetric. Almost any way you cut it in half, the two halves will look the same (it also has smooth borders and only one color). Mole (B) on the right is clearly not symmetric with a bump on the left-hand side, and elongation on the bottom right (it also has irregular borders and multiple shades of brown). I would be concerned about this mole.
Asymmetry is probably the hardest of the ABCDE concepts, but it is one that I like a lot as a clinician. Sometimes a mole has some questionable features but is very symmetric, and that can be reassuring.
Border irregularity refers to the contours of the border. Smooth, regular borders are reassuring. The mole can be circular or oval, but if the borders are smooth all the way around, I take that as a good sign.
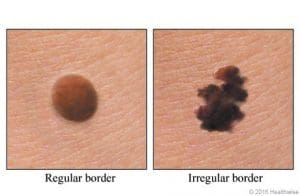
Irregular, jagged, ragged borders are concerning. Mole (D) on the right has obviously irregular borders (along with multiple colors and asymmetry). Asymmetry, along with Irregularity of color and border, tell me that the mole has developed in a disordered fashion, and that is what happens in melanoma, and also can happen in pre-cancerous moles (which we will discuss).

Color refers to how many shades of brown or home many colors (brown, blue, black-red, white) are seen in the mole. One or sometimes two colors (if good symmetry) are reassuring.
Two or more colors with asymmetry is more concerning and again can reflect disordered growth of the mole.
This mole has multiple colors in it: pink, light brown, medium brown, dark brown, and it is asymmetric and slightly irregular borders. It is concerning!
Diameter refers to the width and/or length of the mole. We teach patients that moles over 6 mm are more concerning. In general, larger moles can be more concerning, but without any other features, the diameter is of less concern. What is concerning is a changing diameter, a mole that is growing. Once moles appear and grow, they typically stay the same size (or they may grow with a growing child). This reflects the relative biological inactivity of the mole. If a mole is growing, it means that cells are actively dividing, and the mole is “on the move.” This can be a sign of dysregulation and a concerning sign for melanoma.
Evolution describes a mole that is changing: two months ago it was one color, now it is two colors; it has grown in the past month; there is a new jagged edge to the border. I will always recall a patient from early in my career. She had a mole on her abdomen that had increased in size over the past several months. The mole did not have any other concerning features, but I had been taught that evolution or change was actually the most predictive of melanoma in studies. I tested the mole, and sure enough, it was an early, curable melanoma. Good catch by her (and by me)!
Other concerning features of possible melanomas (and non-melanoma skin cancer), are moles or growths that are bleeding, itching or tender. These are other important reasons to be evaluated by a dermatologist.
Evaluation and Diagnosis
When you come to the dermatologist with a mole of concern, you will get a thorough evaluation. If you are willing, the dermatologist may want to see your other moles in addition to the one that you (or your family member!) has noticed. Sometimes my patients aren’t really aware of their other moles. So when my assistant asks if I can see all your skin, know there is a good reason. The above features are helpful, but sometimes your mole of concern needs to be put into context. Your mole of concern might have two colors, but no other worrisome features. If I look at your 20 moles, and 12 of them look similar, then it lowers my concern a notch, and we can talk about how to monitor them. In general, the more ABCDEs that add up for one mole, the greater the chance we will need to do a biopsy.
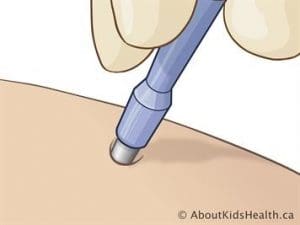
During your visit, you may notice that I, and many of my colleagues, use a lighted magnifier to look at some of your moles. This device, often called a dermatoscope, emphasizes many of the ABCD features for close examination. It allows me to see details of color, pattern and border that may not be apparent with the naked eye. It adds more information to my decision whether to recommend we biopsy the mole.
Biopsy
A concerning mole needs to be biopsied. A biopsy removes some or all of the mole for examination by a dermatopathologist. Thereby, a definitive diagnosis can be made under the microscope. . This is a procedure done under local numbing medicine in the office, often on the same day as your evaluation visit. Most commonly, the mole is removed with a shave biopsy. This leaves a small scoop in the skin, but does not require stitches. If I think there is more depth to the mole, I may recommend a punch biopsy where a small circular cutting tool is used to remove a circular piece of skin. Typically, a couple sutures are placed to help the healing. For a larger, very concerning mole, a small excision may be performed. This is a 20-30 min local procedure in which I cut around the mole with a blade and place underneath dissolving sutures as well as top stitches.


Diagnosis
About a week after the biopsy, I will receive a report from the pathologist telling me about the sample I submitted. Sometimes, happily, it is only a pre-cancerous (or atypical or dysplastic) mole. This means it has some irregular features, but it is not melanoma (yeah!). Some pre-cancerous moles should be removed with stitches to eliminate any chance that the cells can progress to melanoma.
If the report does show a melanoma, that is not the end of the story. Melanomas come in different types and different severities. The prognosis and treatment vary greatly depending on a number of factors. The most important factor for whether the melanoma is of immediate risk to your overall health is the depth of the melanoma. The melanoma report tells me how deep the melanoma goes into the skin. This can vary from a depth of zero, which means the melanoma is only in the top layer of the skin and has no risk of spread; to less than 1 mm, which is an early melanoma and has a very low risk of spread; to deeper melanomas, which do have higher risks of becoming metastatic. Some melanomas are small but deep and dangerous. Some melanomas appear broad on the surface, but they don’t go deep at all. Taking into account the depth and some other factors on the pathology report will allow me to recommend the best treatment.
Treatment
The most important treatment for almost all melanomas is to remove, or excise, the melanoma with a safety margin. This should typically be done within 4-6 weeks of diagnosis. Surgical removal gives the best chance of permanent cure. For most early melanomas under 0.8 mm in-depth, this can be done in the dermatologic surgeon’s office under local numbing medication, and the risk of the melanoma coming back can be 1% or less. While this is a local procedure, it can be a substantial surgery on the skin. Patients usually need to plan for 7-14 days of very light activity as not to damage the healing surgical site. When you have a melanoma removed on the trunk, arms, or legs, you usually end up with a scar to be proud of.
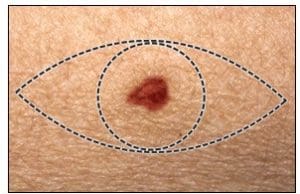
Excision
Let’s take an example of a melanoma on the back. The melanoma was biopsied and found to have a depth of 0.6 mm (great prognosis). The width of the melanoma on the surface was 1.2 cm (that’s half an inch). The recommendation is to remove the melanoma with 1 cm of normal skin all around it. That means the width of the removal (1.2 + 1 + 1) is 3.2 cm. The length of a scar is typically three to four times the width of the area removed. So the scar length would be approximately 10-12 cm (4 to 5 inches).

Sentinel Lymph Node Biopsy (SLNB)
For melanomas deeper than 0.8mm, it is often recommended that the patient have a consultation with a surgical oncologist for a sentinel lymph node biopsy. As the depth of the melanoma increases, so does the risk that melanoma cells may have spread to a nearby lymph node. A SLNB is done by a surgical oncologist under general anesthesia. They inject a dye and a safe radioactive substance at the site of the melanoma and see which lymph nodes it tracks to. The surgeon then goes in and removes the lymph node(s), and at the same time, they do the melanoma removal. If cells are found in a lymph node, there is a higher risk that the cancer can spread, and this information will help determine if any additional surgery or treatment is needed.
Treatment for Melanoma that has Spread
It used to be that metastatic melanoma was frequently fatal. Traditional chemotherapy was not very effective. Things have changed a great deal in the last 10 years with newer therapies targeting specific aspects of the melanoma cells, or those aimed at ramping up the immune system to attack melanoma cells. While melanoma can still be deadly – I recently lost a patient who had presented to me with a very thick advanced melanoma — these can be life-saving treatments for advanced melanoma. In fact, I have an older relative who had metastatic melanoma, was given one of the immune-boosting treatments, and is alive today, five years later.
Bottom Line
The bottom line is that early melanoma is entirely curable with surgery. That is why it is so important that you and your family members have a dermatology evaluation for any suspicious moles or lesions. Some of my patients are hesitant to come into the office during the COVID crisis. Teledermatology is an excellent starting point for evaluating concerning lesions. Some routine growths can be identified, and I can provide reassurance. For worrisome or hard to evaluate growths, we can make a plan for you to safely come into the office for the appropriate biopsy. If you have a mole of concern, please reach out to your primary care doctor or dermatologist so we can figure out how to help.
We’re here to help.